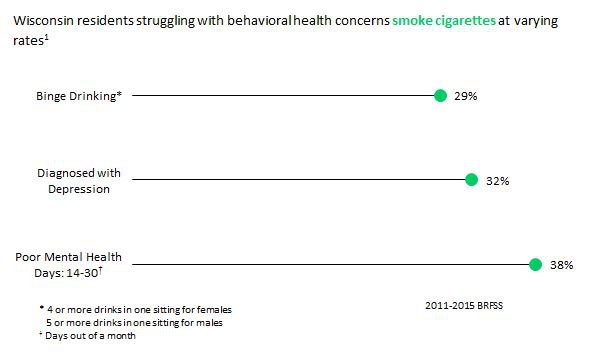
The term "behavioral health" includes both mental illness and substance abuse disorders. In Wisconsin, 16% of residents suffer from mental illness and 26% struggle with substance abuse disorders.1 Opioid users have an extremely high smoking prevalence with estimates/one study finding that 95% of users smoke cigarettes.2 Research has shown that 40% of all cigarettes are smoked by individuals with behavioral health issues.3 Additionally, individuals with multiple marginalized characteristics (e.g., mental illness and low SES) see higher rates of tobacco use. Specifically, 48% of individuals who have a mental illness and live below the poverty line use tobacco.4
Unfortunately, common misconceptions about the relationship between smoking and behavioral health have led to fewer individuals receiving assistance, despite the fact that research shows that when individuals quit tobacco and other substances at the same time, they are 25% more likely to stay off both.5 With a large amount of the behavioral health community smoking, it is important that they receive tailored cessation assistance.
Click here for a powerful video that shows the positive impact of quitting smoking at the same time as quitting other substances.
Individuals who suffer from behavioral health concerns lose about five years of their life (with some studies suggesting it can be up to 20 years) on average compared to individuals without them.6 Studies have shown that individuals with behavioral health concerns may be as much as three times more likely to develop cancer due to late stage diagnosis and inadequate treatment. This may result from behavioral health patients being more likely to receive lower quality of care compared to patients without any concerns.7
It is vital to have a combination of behavioral health treatment and tobacco cessation programs for individuals suffering from mental illness and substance abuse disorders.

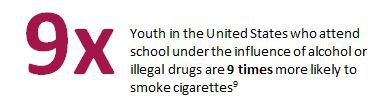
Youth suffering from behavioral health concerns are also more likely to use tobacco than their peers. Youth surveys have shown that 36% of students who attempted suicide and 24% who have purposely hurt themselves without wanting to die (i.e., self-harm) within a year, smoke cigarettes. Youth who use prescription drugs are also six times more likely to smoke cigarettes than drug-free youth.9 Environmental barriers, including social norms, peer influence, and reduced parental monitoring, are large obstacles when promoting smoking cessation resources. Most commonly, children of parents who smoke are more likely to become smokers, so targeting parents in cessation programs can potentially have a positive effect on youth tobacco rates.10
State/Local Resources:
- University of Wisconsin Center for Tobacco Research and Intervention (CTRI)
- The Wisconsin Nicotine Treatment Integration Project (WiNTiP)
- Wisconsin Tobacco Quit Line (800-QUIT-NOW)
National Resources:
- Behavioral Health - What we Know: Information from the CDC on behavioral health and tobacco use
- Health Equity in Tobacco Prevention and Control : Learn more to achieve health equity in tobacco prevention and control
- Smoking Cessation Leadership Center : Understand the components of behavioral health and the importance to quit smoking
- Smoking Cessation for Persons with Mental Illnesses : Explore a toolkit for the best practices for mental health providers
References
- BRFSS (2011-2015 combined dataset)
- "Cigarette Smoking Among Opioid-Dependent Clients in a Therapeutic Community " (2009)
- National Surveys on Drug Use and Health (2009-2011 combined dataset)
- Center for Disease Control and Prevention (2016)
- A Meta-Analysis of Smoking Cessation Interventions with Individuals in Substance Abuse Treatment or Recovery (2004)
- The Tobacco Epidemic Among People with Behavioral Health Disorders (2015)
- Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies (2009)
- Hospital by Public Domain from the Noun Project
- YRBSS 2013 dataset
- Tobacco use in youth with mental illness (2011)